Patients with an EPaCCS form are more likely to die out of hospital
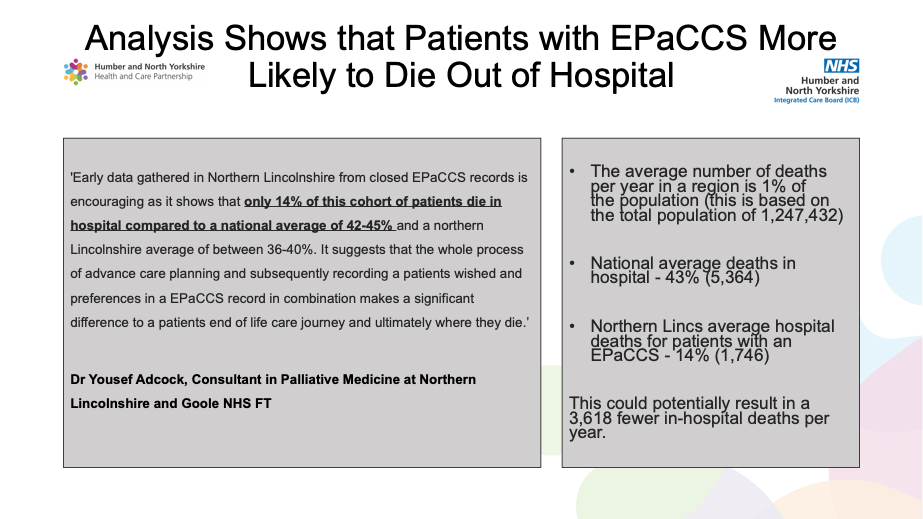
North Lincolnshire, part of Humber and North Yorkshire Integrated Care Board have demonstrated that the use of Electronic Palliative Care Coordination Systems (EPaCCS) with the improved sharing of patient wishes and preferences makes a significant difference to their care. Analysis has shown that deaths in hospitals of patients with an EPaCCS form has fallen to 14% (national average 43%) See diagram 1
HNY had an end goal to improve the co-ordination of care for palliative and End of Life patients and ensure their wishes and preferences were communicated. They teamed up with Black Pear who for many years have delivered software that enables co-ordination of care between all health and social care providers.
The success of EPaCCS across HNY is evidenced by its widespread adoption, with approximately 98% of general practices utilising the system. EPaCCS has garnered support from other healthcare providers, including hospices, ambulance services, community carers, and acute healthcare providers.
HNY’s anticipated benefit of reducing deaths in hospitals of those patients with an EPaCCS form has been realised.